Sources of Error in Monitoring High Speed Testing of Vascular Grafts
Stent Testing
by | RMBS 1998 | Publications, Stent Testing
Sources of Error in Monitoring High Speed Testing of Vascular Grafts
Biomedical Science Instrumentation, 34, pp. 240-245, (1998)
J. C. CONTI,1,2 Ph.D., E. Strope,2 Ph.D., and K. Price2
1 Southwest Missouri State University, Springfield, Missouri
2 Dynatek Dalta Scientific Instruments, Galena, Missouri
RMBS 1998
Keywords
Compliance, tubing, grafts, mechanical, frequency, radial, testing, accelerated, durability, fatigue
Abstract
Mechanical compliance issues are increasingly important in the design, testing, and manufacture of vascular grafts. This has to do with the observed relationship between long-term patentcy of implanted grafts and accurate compliance matching of those devices with the recipient natural vessels. Another important concern in this type of investigation has to do with the use of mock arteries during the testing of implantable medical products such as intravascular stents, stent/grafts, etc. At issue here are not simply the techniques used to monitor the static compliance of the vessels, but the dynamic properties which are in effect during the in vivo utilization of these devices. Perhaps of even more importance is understanding the high speed dynamic properties of these vessels so that a proper and reliable high-speed durability experiment might be designed.
There is a natural tendency to adopt procedures that monitor outside dimensions of the graft or artery. The theoretical problem with this approach is the fact that compliance matching is a phenomenon associated with the inner lumen of the tube, whether it is hydrodynamic considerations in vascular graft testing or loading considerations in stent testing.
Optical techniques such as lasers and ultrasound are encumbered by two physical motion phenomena unique to this approach. The first is simple jumping or movement of the tube due to vibrations. This problem can be overcome by high sampling rates. The second is more problematic and results in lengthening of the tube that has longitudinal as well as radial compliance. Both quantitative and qualitative examples will be examined. A comprehensive understanding of the sources of error encountered in various monitoring techniques is reviewed. These techniques will include lasers, dynamic internal compliance, ultrasound, and cantilevered beams.
Introduction
It has been suggested that there is a need to know and match the internal compliance of vascular grafts in order to optimize their long-term patency [1-6]. A review of the literature indicates a large variation, not only in the experimental design used to evaluate the compliance of both natural vessels and vascular grafts, but also in the techniques that are used to measure these properties. Some of the work was done on excised vessels [7-8] or on natural vessels that are open and exposed to the air [9-10]. Many of the techniques utilize X-rays, and some take advantage of cantilevered beams [11-13] touching the natural vessels or vascular grafts in order to determine the change in diameter versus internal pressure. Another series of experiments reported using various video techniques [14-19].
As investigations into the importance of mechanical compliance expanded it was found that, not surprisingly, the three-dimensional compliance of vascular grafts and mock latex arteries was dependent upon the pulsation rate or testing frequency [20-22]. This information directly affects the design and carrying out of high-speed durability testing on a variety of medical products. At issue is the need to acquire information concerning the long-term fatigue resistance of a compliant product in a short enough period of time to reasonably include this information in standard product development scenarios. Accelerated testing is used in many areas, including metal fatigue analysis and radiation of polymers. By increasing the dose of radiation or the temperature of storage, one can get a certain amount of acceleration in the testing. Those involved in accelerated testing, however, are well aware that there is no perfect accelerated test that does not include some problems associated with the higher load stress levels, whether it be from temperature, radiation, or physical loading. This type of scenario requires a thoughtful and comprehensive approach to the evaluation of variables that can introduce complications into an experiment and result in less reliable final data.
In vascular graft or mock artery testing at high frequencies or pulsation rates, one area of concern is how the motion of the graft responds to increasing the rate of testing. The key to understanding these frequency dependent changes in mechanical properties has to do not only with an awareness that these properties can change but also a careful choice of experimental protocols and instrumentation that give a clear understanding of how properties are changing at faster rates.
It is the overall goal to test long-term durability and fatigue properties of a product as fast as possible so as to reduce the amount of time it takes to get important information to support government submissions or product design changes early enough in the cycle to contribute effectively to the final design of the product, yet not so fast that the experiment becomes unreliable. The general goal should be to neither overstress or understress the product in the process of accelerated testing. Overstressing can lead to unpredicted or unjustified product failure and may result in the tendency to ignore failures that occur. This can, of course, be devastating if the failures do, in fact, reflect problems with the performance of the product. On the other hand, an understressed product has the obvious disadvantage of producing unjustified confidence in the long-term durability properties of the product. It can also lead to later in vivo failures that can be devastating to both the patient and the manufacturer.
We will evaluate different techniques used to determine the compliance of vascular grafts and share experiences and concerns that we have with monitoring techniques that, if improperly used, could result in unreliable data that reduces the validity of the related testing program.
General Considerations
There are several straightforward issues that should be mentioned first. Clearly, all transducers need to be properly chosen and calibrated to give reliable data with a defined precision and accuracy matched to the need of the experiment. One common problem in scientific literature is recording data from a transducer whose precision is not reported. As a result, an ultrasonic measurement that is plus or minus 0.2mm in precision would be incapable of delivering reliable data on a 5mm vascular graft with a compliance of 0.5% per 100mm Hg.
It is important to realize the magnitude of these dimensions in order to understand the accuracy and precision of the measuring device. The magnitude of the problem can be demonstrated with a simple calculation. As an example, we are working with a vascular graft with an internal radial compliance of 3% per 100mm Hg (or 1.2% per 40mm Hg) and an internal diameter of 4mm. This is very typical of vascular grafts currently under investigation. In order to calculate the change in internal radius, Δr, of the graft over an 80-120mm Hg pressure excursion, we use:
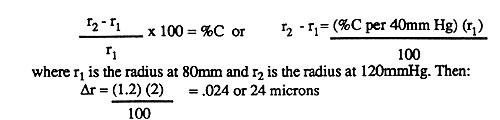
As can be seen, we are dealing with relatively small amounts of change in position, and therefore appropriate accuracies and precisions must be considered.
Another obvious concern is the nature of the in vitro experimental solution. Although usually reported, the chemical nature of the solution as well as the temperature should be recorded. This would require some understanding of the accuracy and precision of the temperature measuring devices.
External Compliance
In general, the concept of matching compliance of vascular grafts for implantation purposes specifically refers to the inner luminal walls of the graft. Therefore, an understanding of the internal compliance of the vessel is most important. A red blood cell or a platelet shooting through the vasculature along the lumen of a vessel comes upon an anastamosis and a vascular graft that is slightly less compliant. As a result, turbulence will develop at this anastamosis, platelets will be activated and deposited, and the clotting cascade will continue. A similar situation is the use of mock arteries to test various devices to be delivered to the vasculature. Again, these devices are all in contact with the inside of the graft. Therefore, the position of the lumen versus pressure or internal compliance is the important parameter.
Although internal measurements are more difficult than external measurements, the following calculation will illustrate the necessity of internal measurements. In order to understand the relationship between internal and external compliance, the wall thinning that occurs as a tube expands must be understood. In this example, assume a 4mm latex graft with an internal compliance of 3% per 100mm Hg and a wall thickness of 0.050 inches or 1.27mm. This results in an external diameter of 6.54mm. As the graft increases in diameter by internal pressurization from 80-120mm Hg, then the following analysis will illustrate the error associated with wall thinning.
Consider a ring with an inside diameter (i.d.) of 4mm, an outside diameter (o.d.) of 6.54mm, and a wall thickness of 1.27mm (.050″). This analysis uses cross-sectional areas since the length factor converting area to volume in this example would be a constant. The cross-sectional area of this ring will be given by:
π ro2 – π ri2 = Area
where ro is the radius of the outer part of the ring and ri is the radius of the inner part. Then,
Cross-sectional area of the wall = 33.58mm2 – 12.56mm2 = 21.02mm2
Upon expansion, the cross-sectional area of the ring would have to be a constant to obey the conservation of mass laws. This assumes the tube does not lengthen and the wall itself does not compress. Therefore, when going from 80 to 120mm Hg (ignoring the initial expansion from 0 to 80mm Hg) the inner lumen changes from a diameter of 4mm to a diameter of 4.048mm (see earlier example). Therefore:
A80 = A120 = 21.02mm2 = π ro2 – π ri2
21.02mm2 + π ri2 = π ro2
33.86 = π ro2
or ro = 3.283 and the new outside diameter is 6.566mm.
In this analysis, the o.d. is 6.566 and not the 6.588 predicted if both the inner lumen and outer lumen moved the same amount. The 22 microns represents about a 46% error (22/48 x 100) when interpreting uncorrected wall movement. The above example addresses only wall thinning and not the larger problem of wall compression in graft designs that are porous in nature.
Another major problem with monitoring external diameter of vascular grafts during high speed testing has to do with simple vibrations. Since nearly all of the devices used to test the accelerated durability of vascular grafts have, by requirement, moving parts that are pumping fluid, there is a natural tendency to have vibration in the instrument. The amount of vibration is a function of several factors such as the design of the instrument, the experimental bench holding the instrument, and the nature of the laboratory floor. In our laboratory it is not uncommon to have movement of the graft on the order of 8-10 microns with each pulse. Adding this to the above 22 micron error, we could have a total of 30-32microns of error. This translates to a % error of 31/48 x 100 or 65%. This vibration alone would represent 18% error in the above example.
A final problem with external measurements has to do with the fact that most grafts that have radial compliance also have some longitudinal compliance. This means that as the pressure is increased inside of the vascular graft, not only will the diameter increase, but the graft will also get longer. This lengthening will cause a temporary “drooping” in the graft on an experimental apparatus, changing its position in space temporarily. The magnitude of the drooping is quite surprising, as can be shown in following calculations. Assume a 10cm long vascular graft of 4mm diameter and 3% per 100mm Hg radial compliance. Also assume 1/100th as much longitudinal compliance, or 0.03% per 100mm Hg. This is representative of many of current products. Over a 40mm Hg excursion, such a sample would stretch about 12 microns, resulting in a 30-36 micron droop. This is the same order of magnitude as the combined errors from wall thinning and vibration described above.
The accuracy of ultrasonic techniques in a dynamic system have, in our hands, been somewhat problematic. Review of the above calculations shows this kind of precision and accuracy can often lead to a 100% or more error in our measurements. In addition, ultrasonic techniques require nearly perfect alignment of the crystals and can be plagued by slow systemic response time. Systemic response time does not refer to the actual transit speed of the sound or the processing speed of the data, but the speed at which the system itself can update the data coming back.
Another common technique which we use in our laboratory is laser determination of the external diameter of the vessels versus time. At first inspection, lasers appear to be a perfect way to do this evaluation. However, it is important to realize that there are many reasonably priced laser systems with response times that are too slow to determine precisely external diameters with devices that are pulsing at 30, 40, or 50 Hz. One of the best ways to check this accuracy is to cross-check it with an internal compliance measurement. The laser systems that we currently use are highly precise (0.01mm) but have problems at testing speeds above 4 or 5 Hz. We are currently evaluating a 200Hz laser system which may solve some of the above problems. A final technique that seems promising is the use of high-speed video photography to capture the external dimensions of the graft at different points in the cycle. Although not plagued by the precision problems previously discussed, this measurement does not look at the three-dimension properties of the graft, but is only looking at the graft on a two-dimensional plane. Symmetry in the expansion of the graft must be assumed, as it is with laser and ultrasonic systems as well.
Internal Compliance
Most errors found in external compliance measurements are eliminated when internal compliance is used. We have used internal compliance measurements for over ten years and have reported some of these results [20-22]. To evaluate the internal compliance of a tube, the initial length and inside radius of the tube at atmospheric pressure must be measured. This can be done using machinist’s pins. The initial volume of the rod that represents the inside lumen of the graft will be:
Vi lumen = πri2 li
where ri= initial radius
li = initial length
If the tube is then inflated to some pressure p, a new set of dimensions results if the tube has any compliance. The new volume would be:
Vp = π rp2 lp
so that the change in volume from the initial state to the higher pressure state will be:
Vp – Vi = ∆V =π rp2 lp–π ri2 li
or (∆V /π) = rp2 lp-ri2 li
Since the initial dimensions and the change in volume are measurable, then:
(∆V /π) + ri2 li = rp2 lp
If the change in length is measurable, then:
((∆V / π) + ri2li) / lp = rp2 or rp = (((∆V / π) + ri2li) / lp)1/2
where rp is the new radius. For the purpose of convention, we normalize all results to a 100mm Hg increase in pressure so that:
( (rp-ri) / ri ) x (100 / ∆P) x 100 = % radial compliance
or ( (rp-ri) / ri ) / ∆P x 104 = % radial compliance
where ∆P is expressed in mm Hg. (Note: The formulas for dynamic compliance at subcritical speeds are identical to those for static determinations.) To determine the high speed properties of a vessel after the initial compliance is determined at 72bpm, one simply turns up the speed of the test while constantly monitoring the compliance of the vessel.
One source of error in the internal compliance measurement is similar to the assumption of symmetry with all of the optical techniques. That is, the vessel is assumed to be homogeneously compliant both radially and longitudinally. This can be tested in many cases by determining the reproducibility of the data from point to point. For example, one can take a 10cm long graft and measure its dynamic internal compliance, cut the graft into shorter and shorter pieces (for instance, 0.25cm at a time), and determine how the internal compliance varies throughout this experiment. A consistent compliance would indicate homogeneous properties.
A static measurement is simply a poorly defined dynamic measurement. Many vessels, whether natural vessels, polyurethane, silicone, or latex, all have frequency versus compliance relationships that are surprisingly close to each other. After switching from static to dynamic mode, the properties of these grafts all remain fairly constant up to a speed of approximately 1200bpm. At some frequency above 1200bpm, there will be a sudden reduction in compliance. This is related to the frequency at which the walls of the tube can no longer respond to the dynamic pressure changes. If the walls cannot follow the pressure excursion, appropriate mechanical work is not experienced by the walls of the device. Either the speed of test must be decreased, or the experimental design might be modified to overpressurize the system to account for the reducing compliance. This overpressurization, although allowing faster testing, will require overloading of the product, which may lead to a dead end if product failure occurs during this testing.
As with all experimentation, a clear understanding of the sources of error in the long run results in greater reliability in the data from the experimentation.
References
1. Kinley, C. E., and Marble, A. E., Compliance. J. Cardiovasc. Surg., 21, 163-170 (1980).
2. Clark, R. E., Apostolou, S., and Kardos, J. L., Mismatch of Mechanical Properties as a Cause of Arterial Prosthesis Thrombosis. Surg. Forum, 27, 208-217 (1976).
3. Gonza, E. R., Mason, W. F., Marble, A. E., and others, Necessity for Elastic Properties in Synthetic Arterial Grafts. Can. J. Surg., 17, 176-179 (1974).
4. Lyman, D. J., Fazzio, F. J., Voorhees, H., and others, Compliance as a Factor Effecting the Patency of Copolyurethane Vascular Grafts. J.
Biomed. Master. Res., 12, 337-339 (1978).
5. Abbott, W. M., and Bouchier-Hayes, D. J., The Role of Mechanical Properties in Graft Design. In: Graft Materials in Vascular Surgery. Edited by H. Dardik. Miami: Symposia Specialists, Inc., 59 (1978).
6. Baird, R. N., Kidson, I. G., L’Italien, J. G., and Abbott, M. W., Dynamic Compliance of Arterial Grafts. Am. J. Physiol., 2, 568-572 (1977).
7. Bergel, D. H., The Static Elastic Properties of the Arterial Wall. J. Physiol. (London), 156, 445 (1961).
8. Bergel, D. H., The Dynamic Elastic Properties of the Arterial Wall. J. Physiol. (London), 156, 448 (1961).
9. Patel, D. J., De Freitan, F. M., Freenfield, J. R., and Fry, D. L., Relation of Radius to Pressure Along the Aorta in Living Dogs. J. Appl. Physiol, 18, 1111 (1963).
10. Paterson, L. H. Jensen, R. E. and Parnell, J., Mechanical Properties of Arteries In Vivo. Circulation Res., 8, 622 (1960).
11. Walden , R., L’Italien, G. J., Megerman , J., and A bbott , W. M., Matched Elastic Properties and Successful Arterial Grafting. Arch. Surg., 115, 1166-1169 (1980).
12. Gow, B. S., and Taylor, G., Measurement of Viscoelastic Properties of Arteries in the Living Dog, Circulatory Research, 23, 111 (1968).
13. Gow, B. S., An Electrical Caliper for the Measurement of Pulsatile Arterial Diameter In Vivo. J. Appl. Physiol, 21, 1122 (1960).
14. Gotoh, F., Muramatsu, F., Fukuuchi, Y., Okaysu, H., Tanaka, K., Suzuki, N., and Kobari, M., Video Camera Method for Simultaneous Measurement of Blood Flow Velocity and Pial Vessel Diameter. J. Cereb. Blood Flow Metab.,
2, 421-428 (1982).
15. Assmann, R. and Henrich, H., A Video-Angiometer for Simultaneous and Continuous Measurement of Inner and Outer Vessel Diameters. Pflugers Arch., 376, 263-266 (1978).
16. Halpern, W., Mongeon, S. A., and Root, D. T., Stress, Tension and Myogenic Aspects of Small Isolated Extraparenchymal Rat Arteries. In: Smooth Muscle Contraction, edited by N.L. Stephens. New York : Dekker, 427-456 (1984).
17. Intaglietta, M. and Tompkins, W. R., On-Line Measurement of Microvascular Dimensions by Television Microscopy. J. Appl. Physiol., 32, 546-551 (1972).
18. Wiederhielm, C. A., Continuous Recording of Arteriolar Dimensions with a Television Microscope. J . Appl. Physiol., 18, 1041-1042 (1963).
19. Halpern, W., Osol, G., Coy, G. S., Mechanical Behavior of Pressurized In Vitro Prearteriolar Vessels Determined with a Video System. Annals of Biomedical Engineering, 12, 463-479 (1984).
20. Conti, J. C., Strope, E. R., Rohde, D. R. and Greisler, H. P., A New Technique to Determine Vascular Compliance In Vivo, National Heart Lung and Blood Institute Contractors Meeting. Louisville, KY, 1989.
21. Bozzi, R., Conti, J. C., Soldani, G., Spence, L., Strope, E., and Withrow, D., Relating the Frequency Dependent Radial Compliance to the Tensile Modulus of Polyurethane and Latex Vascular Grafts. Transactions 5th World Biomaterials Congress, 434, U2 (1996).
22. Conti, J. C., Strope, E. R., Rohde, D. J., and Spence, L. D., Frequency Dependent Radial Compliance of Latex Tubing. Biomedical
Sciences Instrumentation, 33, 524-529 (1997).



