Frequency Dependent Hysteresis of Silicone and Latex Mock Arteries Used in Stent Testing
Mock Artery Compliance
by | RMBS 2005 | Publications, Compliance, High Speed Photo, Silicone Mock Arteries
Frequency Dependent Hysteresis of Silicone and Latex Mock Arteries Used in Stent Testing
Ramesh Rajesh1, Strope ER2, Price KS2, Conti JC3
1 University of Kansas, Department of Mechanical Engineering, Lawrence, KS 66046
2 Dynatek Dalta Scientific Instruments, 105 E Fourth St, Galena, MO 65656
3Department of Physics, Astronomy and Material Sciences, Southwest Missouri State University, Springfield, MO 65803
RMBS 2005
Keywords
Compliance, Latex, Silicone, Artery, Frequency, Hysteresis, Stent, Testing, Vessels
Abstract
Mock arteries also called as mock vessels are one of the best alternatives available to researchers in evaluating the mechanical characteristics and durability of intravascular medical products without having to use animal and human clinical studies. The behavior of mock arteries depends on the frequency of loading. This makes it essential to evaluate and analyze the compliance and hysteresis of the mock arteries at different frequencies. Hysteresis, the difference in the pressure-volume curve between the loading cycle and the unloading cycle, plays an important role in determining the mechanical properties of the mock arteries. Six each of silicone and latex mock arteries were tested for this study. Three silicone and three latex mock arteries were tested at room temperature for dynamic internal compliance, and the remaining three each of silicone and latex mock arteries were soaked in distilled water at 37° C for 36 hours and then compliance tested using a dynamic compliance tester. All arteries were tested at four different frequencies: 72, 500, 1000, and 1500 beats per minute.
Results showed that as the frequency is increased, the area of the hysteresis curve increased and the compliance of the tube decreased. This was clearly evident in both silicone and latex mock arteries. Latex mock arteries had more hysteresis compared to silicone mock arteries. The compliance of only the latex mock arteries was affected by soaking in distilled water; the compliance of silicone mock arteries did not change. Latex mock arteries showed higher compliance than silicone mock arteries in either the soaked or unsoaked condition.
Introduction
Evaluation of mechanical characteristics of intravascular medical products has made it necessary for the researcher to conduct animal studies. Mock arteries used in medical device testing have proven to serve as an alternative to using animals in device evaluation studies. Earlier work has shown that biological vessels have radial compliance in the range of 4-7 % [1-4]. The silicone and latex mock arteries used in this study were selected based on this criterion. Radial compliance of a mock artery depends on the radius of the artery and internal pressure to which it is pulsed and plays a very critical role during in vitro experiments. Currently, mock arteries are tested for compliance according to standards set by AAMI/ISO [5], which suggests testing mock arteries a frequency of 60 ± 10 Hz to simulate real time loading conditions. If the radial compliance and hysteresis of mock arteries were to be investigated successfully at higher frequencies then it opens the door for an option of testing the mock arteries at increased frequency, effectively reducing the time span of the durability testing of intravascular products such as stents.
This paper will present an analysis of the change in area of the hysteresis curve and change in compliance of mock arteries in accordance with change in frequency of testing. In addition, the study will also make a comparison between the silicone and latex mock arteries tested in two different conditions (dry and wet).
Methods
Six silicone and six latex mock arteries were used for this study. External/internal diameter and wall thickness of the mock arteries were measured using a Laser Mike 183. From each group of silicone or latex mock arteries, three were soaked in distilled water for 36 hours at 37°C. External/internal diameters and wall thickness for these wet mock arteries were measured again. All 12 mock arteries were tested on a dynamic compliance tester for radial compliance. The dynamic compliance tester is equipped with a speed controlled motor that turns a shaft on which an adjustable eccentric coupler is mounted. The coupler, along with a crank arm converts the rotational motion into linear motion, which moves a drive rod that compresses a bellows. The drive rod is connected to a highly sensitive linear voltage displacement transducer (LVDT). During the test setup, one end of the mock artery is fixed to the discharge end of the bellows and the other end is mounted vertically to a manifold where a pressure transducer is fixed. The operation of this instrument is quite simple. The volume of the fluid injected into the mock artery is monitored by the LVDT. This LVDT monitors the position of the drive rod, which in turn determines the amount of fluid being injected from the bellows. Pressure is monitored by the pressure transducer and length change is monitored but neglected since the magnitude is so small. All the test data were acquired and recorded on a computer using a LabVIEW data acquisition system.
Testing: The dynamic compliance tester was calibrated for pressure and volume. A mock artery was mounted on the testing machine by means of clamps, which helps in preventing the slippage of the specimen during testing. Length of the mock artery was fixed to ensure that the specimen maintains the original length and has enough longitudinal tension to prevent buckling. The artery was then filled with CP solution (mixture of ProClin and distilled water) and the motor was started at a pulse rate of 72 bpm, while the amount of fluid injected and internal pressure of the system was simultaneously monitored. The stroke length of the system was adjusted such that the maximum and minimum pressure varied between 0 and 120mm Hg. Data was recorded under these conditions and then the motor speed was increased to 500 bpm and data was again recorded. This process was repeated for 1000 and 1500 bpm. All data were analyzed for % radial compliance between 80 and 120mm Hg.
Data obtained from the dynamic compliance tester (pressure and change in volume) were used to plot a graph of loading and unloading curves. A second order polynomial curve was used to get the curve of best fit. The equation of the polynomial curve of best fit was used to determine the area under the loading and unloading curves by means of integration by Simpson’s 1/3 rd rule and also by the Trapezoidal rule. The units of the hysteresis curve were pressure (mm Hg) × change in volume (mm3).
Principle of Measuring Radial Compliance:
To determine the radial compliance of the tube (mock artery), the initial length (Li) and the initial radius(Ri) of the tube has to be measured; in other words, initial volume (Vi) of the tube has to be determined.
Vi = Π ×Ri2 ×Li
Vi is the volume at 0 mm Hg pressure.
If the tube is then inflated to a new pressure P2 with the length being fixed (there is minimal change in length Li), a new set of dimensions results for the tube depending on its compliance. Let ∆V be the change in volume; therefore, final volume Vf of the tube at pressure P2 is given by:
Vf = Vi +∆ V
Vf = Π × Rf2×Li (where Rf is the radius at pressure P2)
Rf = sqrt (Vf / (Π ×Li))
% radial compliance is given by ((Rf-Ri) / (Ri × ∆P)) × 104
where ∆ P is change in pressure expressed in mm Hg.
RESULTS
External/internal diameters and wall thickness of mock arteries were measured with a Laser Mike 183.
Table 1: External/internal diameters and thickness of mock arteries
| * All measurements in mm | |||
| Latex Mock Arteries-Dry | |||
| ID | OD | Thickness | |
| Tube # 1 | 10.802 | 13.585 | 1.391 |
| Tube # 2 | 11.189 | 14.143 | 1.477 |
| Tube # 3 | 11.402 | 14.426 | 1.512 |
| Tube # 4 | 11.498 | 14.437 | 1.469 |
| Tube # 5 | 11.545 | 14.427 | 1.441 |
| Tube # 6 | 11.441 | 14.372 | 1.466 |
| Latex Mock Arteries- Wet | |||
| Tube # 1 | 11.149 | 14.058 | 1.454 |
| Tube # 2 | 11.625 | 14.713 | 1.544 |
| Tube # 5 | 12.062 | 15.059 | 1.498 |
| Silicone Mock Arteries- Dry | |||
| Tube # 1 | 10.745 | 13.233 | 1.243 |
| Tube # 2 | 10.656 | 13.134 | 1.239 |
| Tube # 3 | 10.637 | 13.200 | 1.281 |
| Tube # 4 | 10.677 | 13.226 | 1.274 |
| Tube # 5 | 10.645 | 13.146 | 1.250 |
| Tube # 6 | 10.691 | 13.090 | 1.199 |
| Silicone Mock Arteries- wet | |||
| Tube # 1 | 10.838 | 13.271 | 1.216 |
| Tube # 2 | 10.867 | 13.235 | 1.184 |
| Tube # 6 | 10.868 | 13.155 | 1.143 |
Table 2: Silicone mock arteries
| Silicone Mock Arteries Wet: | ||||||
| Sample length (mm) | Frequency (bpm) | % Compliance | Area under loading curve | Area under unloading curve | Area between Curves | |
| Tube # 1 | 84 | 72 | 5.42 | 56786.4 | 49745.8 | 7040.6 |
| 500 | 5.17 | 60249.1 | 49568.9 | 10680.2 | ||
| 1000 | 4.97 | 53304.2 | 35416.8 | 17887.4 | ||
| 1500 | 3.70 | 52404.7 | 30935.6 | 21469.1 | ||
| Tube # 2 | 89 | 72 | 5.07 | 57248.2 | 50185.2 | 7063.0 |
| 500 | 4.84 | 55059.0 | 44805.5 | 10253.5 | ||
| 1000 | 4.40 | 56420.1 | 38980.5 | 17439.6 | ||
| 1500 | 4.07 | 54043.3 | 32970.0 | 21073.3 | ||
| Tube # 6 | 89 | 72 | 4.92 | 57448.9 | 50150.9 | 7298.0 |
| 500 | 4.77 | 56433.0 | 46305.9 | 10127.1 | ||
| 1000 | 4.52 | 55769.7 | 37937.0 | 17832.7 | ||
| 1500 | 3.89 | 52071.4 | 30519.0 | 21552.4 | ||
| Silicone Mock Arteries Dry: | ||||||
| Tube # 3 | 81 | 72 | 4.94 | 55375.7 | 49826.8 | 5548.9 |
| 500 | 4.78 | 49521.1 | 41858.3 | 7662.8 | ||
| 1000 | 4.41 | 43643.5 | 31875.0 | 11768.5 | ||
| 1500 | 3.58 | 45198.6 | 30725.6 | 14473.0 | ||
| Tube # 4 | 82 | 72 | 4.91 | 54291.1 | 48567.8 | 5723.3 |
| 500 | 4.86 | 55854.9 | 48113.7 | 7741.2 | ||
| 1000 | 4.72 | 45381.2 | 33919.7 | 11461.5 | ||
| 1500 | 3.72 | 45293.8 | 31300.7 | 13993.1 | ||
| Tube # 5 | 82 | 72 | 4.96 | 58147.3 | 52382.1 | 5765.2 |
| 500 | 4.92 | 53724.0 | 46424.5 | 7299.5 | ||
| 1000 | 4.51 | 46351.0 | 34836.6 | 11514.4 | ||
| 1500 | 3.62 | 47010.2 | 33095.6 | 13914.6 | ||
Table 3: Latex mock arteries.
| Latex Mock Arteries Wet: | ||||||
| Sample length (mm) | Frequency (bpm) | % Compliance | Area under loading curve | Area under unloading curve | Area between Curves | |
| Tube # 1 | 90 | 72 | 6.54 | 96508.7 | 84031.3 | 12477.4 |
| 500 | 6.27 | 86243.1 | 71867.5 | 14375.6 | ||
| 1000 | 6.18 | 76911.0 | 57336.9 | 19574.1 | ||
| 1500 | 5.56 | 76315.7 | 50337.1 | 25978.6 | ||
| Tube # 2 | 88 | 72 | 6.71 | 96367.8 | 83844.2 | 12523.6 |
| 500 | 6.59 | 86180.1 | 71435.5 | 14744.6 | ||
| 1000 | 6.47 | 78254.1 | 59166.3 | 19087.8 | ||
| 1500 | 5.27 | 79417.0 | 53415.9 | 26001.1 | ||
| Tube # 5 | 83 | 72 | 7.45 | 114843.0 | 100684.0 | 14159.0 |
| 500 | 7.15 | 102749.0 | 85056.0 | 17693.0 | ||
| 1000 | 7.11 | 103540.0 | 79203.9 | 24336.1 | ||
| 1500 | 5.64 | 79032.8 | 52514.6 | 26518.2 | ||
| Latex Mock Arteries Dry: | ||||||
| Tube # 3 | 76 | 72 | 5.03 | 58935.6 | 52704.1 | 6231.5 |
| 500 | 5.01 | 53278.8 | 43963.3 | 9315.5 | ||
| 1000 | 2.83 | 52946.1 | 38777.4 | 14168.7 | ||
| 1500 | 1.37 | 53635.6 | 32518.1 | 21117.5 | ||
| Tube # 4 | 78 | 72 | 5.07 | 61129.3 | 55187.2 | 5942.1 |
| 500 | 5.05 | 51301.5 | 42100.4 | 9201.1 | ||
| 1000 | 2.35 | 47809.4 | 33191 | 14618.4 | ||
| 1500 | 1.66 | 54570.1 | 33249.9 | 21320.2 | ||
| Tube # 6 | 76 | 72 | 5.04 | 59740.6 | 53272.8 | 6467.8 |
| 500 | 4.90 | 50984.7 | 41966.9 | 9017.8 | ||
| 1000 | 2.67 | 48675.5 | 34062.0 | 14613.5 | ||
| 1500 | 1.81 | 53372.0 | 32172.9 | 21199.1 | ||
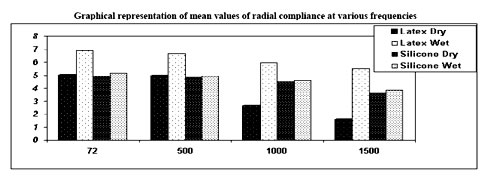
Table 4: Mean and standard deviation of compliance of mock arteries at various frequencies
| Frequencies | Latex Mock Arteries Dry | Latex Mock Arteries Wet | Silicone Mock Arteries Dry | Silicone Mock Arteries Wet |
| 72 | 5.04 ± 0.020 | 6.90 ± 0.483 | 4.93 ± 0.025 | 5.13 ± 0.256 |
| 500 | 4.98 ± 0.076 | 6.67 ± 0.445 | 4.85 ± 0.070 | 4.92 ± 0.213 |
| 1000 | 2.61 ± 0.244 | 5.97 ± 0.626 | 4.54 ± 0.158 | 4.63 ± 0.300 |
| 1500 | 1.61 ± 0.223 | 5.49 ± 0.194 | 3.64 ± 0.072 | 3.88 ± 0.185 |
DISCUSSION
In evaluating the properties of mock arteries, it is essential to monitor the compliance and hysteresis at all pertinent frequencies.
Table 1 shows the geometrical parameters measured by the Laser Mike® 183 for mock arteries. From this it is evident that when the mock arteries (both silicone and latex) are soaked for 36 hours at 37°C there was change in diameter (both internal and external) and also the wall thickness. Latex arteries showed more change in dimensions when compared to silicone mock arteries; in other words, latex mock arteries have more tendencies to absorb water and swell when compared to silicone mock arteries. This hydrophilic nature of latex is not a good characteristic of mock arteries since a change in diameter changes the radial compliance of mock arteries and both properties are important in in vitro testing.
Tables 2 and 3 show the compliance and the hysteresis characteristics of latex and silicone mock arteries with respect to change in testing frequencies. It is evident from the results that both silicone and latex mock arteries, when tested under dry condition at 72 bpm have a compliance value of nearly 5%. As the frequency was increased from 72 bpm the radial internal compliance of mock arteries decreased. In the case of latex mock arteries the compliance decreased from 5.04 ± 0.020% at 72 bpm to 1.613 ± 0.223% at 1500 bpm, which corresponds to approximately 68% decrease in compliance. In the case of silicone mock arteries, radial compliance decreased 4.93± 0.025% at 72 bpm to 3.64 ± 0.072% at 1500 bpm, which corresponds to approximately 26% decrease in compliance. The hysteresis was larger for the wet latex tubes by a factor of 1.8 at 72 bpm and 1.3 at 1500 bpm than the silicone tubes. The hysteresis of the dry latex tubes was larger by a factor of 1.09 at 72 bpm and 1.5 at 1500 bpm than the silicone tubes.
In the case of water soaked mock arteries, compliance also decreased as the frequency increased. In the case of latex mock arteries the radial compliance was 6.90 ± 0.484% at 72 bpm which corresponds to 36% more compliance when compared to latex mock arteries tested in dry condition, and this decreased as the frequency increased to 5.49 ± 0.195% at 1500 bpm. Water soaked silicone mock arteries behaved similar to dry silicone mock arteries with compliance being 5.14 ± 0.26% at 72 bpm corresponding to 4% increase in compliance, compared to silicone mock arteries tested in dry condition and this decreased to 3.89 ± 0.185% at 1500 bpm.
CONCLUSION
The purpose of this study was to evaluate the effect of frequency on the compliance and hysteresis of dry and hydrated silicone and latex mock arteries. The results indicate that silicone is superior to latex in its ability to maintain initial mechanical properties at elevated testing frequencies. Further investigations are ongoing.
ACKNOWLEDGMENTS
Special thanks to all the employees of Dynatek Dalta Scientific Instruments.
REFERENCES
1) Conti, J.C. and Strope, E.R., Radial Compliance of Natural and Mock Arteries: How this Property Defines the Cyclic Loading of Deployed Vascular Stents. Biomedical Sciences Instrumentation, 38, 163-171, (2002)
2) Conti, J.C., Strope, E.R., Rhode, D.J. and Spence, L.D., Frequency Dependent Radial Compliance of Latex Tubing. Biomedical Sciences Instrumentation, 33, 524-529 (1997)
3) Conti, J.C., Strope, E.R., Rohde, D.R. and Greisler, H.P., A New Technique to Determine Vascular Compliance In Vivo, National Heart Lung and Blood Institute Contractors Meeting. Louisvelle, KY, 1989
4) Gonza, E.R., Mason, W.F., Marble, A.E., and others, Necessity for Elastic Properties in Synthetic Arterial Grafts. Can. J. Surg., 17,176-179 (1974)
5) AAMI/ISO standard ISO/CD- V-1 25539-01:2003 and ANSI/AAMI VP-20, 1994



